Cancer treatment, particularly chemotherapy, is a formidable journey for patients and healthcare providers alike. While advancements in medical science have improved outcomes, the process of chemotherapy comes with its own set of challenges.
From medication delivery to managing side effects, ensuring effective chemotherapy care demands a comprehensive approach. In this article, we explore the intricacies of navigating these challenges and optimizing the chemotherapy experience for patients.
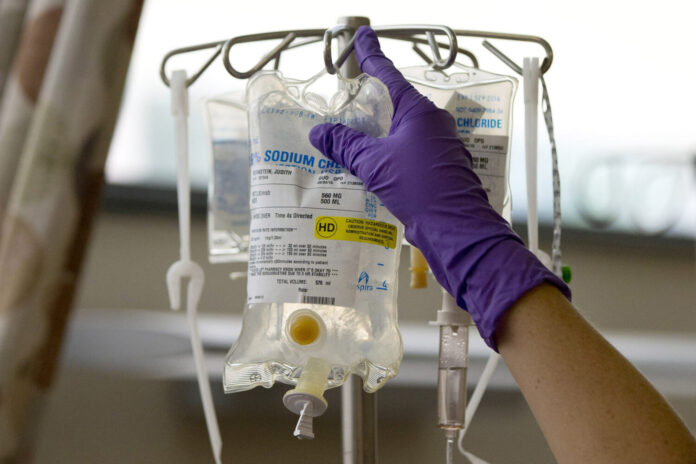
The Importance of Precision in Medication Delivery
Precision in chemotherapy medication delivery is critical for treatment success. Healthcare providers meticulously calculate and administer chemotherapy doses to ensure therapeutic agents reach their intended targets while minimizing damage to healthy tissues.
Intricate protocols and cutting-edge technologies, such as infusion pumps and automated dosage systems, enable precise delivery, reducing the risk of under or overdosing. The emphasis on precision enhances treatment efficacy and minimizes adverse effects, contributing to a more targeted and personalized approach to cancer care.

Addressing Adverse Reactions and Side Effects
Chemotherapy often triggers a range of side effects, from nausea and fatigue to more severe complications. According to Cancer.Net, blood disorders, and nervous system effects are some of the more serious side effects of chemotherapy. Effective management of these reactions requires a personalized approach, with healthcare teams tailoring interventions to the specific needs of individual patients.
Antiemetic medications can alleviate nausea, and supportive therapies such as acupuncture or counseling may mitigate fatigue and emotional distress. Regular communication between healthcare providers and patients allows for timely adjustments to treatment plans, fostering a collaborative environment that prioritizes patient comfort and well-being.
Enhancing Patient Education and Empowerment
Empowering patients with knowledge about their treatment is crucial. Comprehensive education on the chemotherapy process, potential side effects, and self-care measures equips individuals to actively participate in their care. This promotes a sense of control and reduces anxiety.
Healthcare providers should encourage open communication, providing resources such as pamphlets, videos, or online platforms where patients can access reliable information.
According to The Pharmacist, only one-third of patients fully understand the patient information leaflet (PIL) that comes with their medication. According to a survey, less than half of those who responded read it. Pharmacists can help by participating in pilot projects that evaluate innovative methods of providing medication information to patients.
Well-informed patients are better positioned to make decisions about their treatment, adhere to medication schedules, and engage in practices that promote overall health.

Technological Innovations for Treatment Monitoring
In the digital age, technology plays a crucial role in improving chemotherapy care. Remote monitoring tools allow healthcare providers to track patient progress, identify issues early, and adjust treatment plans promptly, enhancing overall treatment efficacy.
Wearable devices and smartphone applications enable patients to report symptoms in real-time, facilitating timely interventions. Telehealth consultations provide a convenient means for patients to connect with their healthcare team, fostering continuous communication and support.
Adopting these technological innovations enhances the efficiency of chemotherapy care, making it more patient-centric and adaptable to individual needs.
Implantable Catheter Devices for Medication Delivery
Implantable catheter devices play an important role in optimizing chemotherapy precision. These devices, often surgically implanted, provide a direct conduit for delivering therapeutic agents, ensuring precise administration while minimizing the impact on surrounding tissues. Educating patients about the purpose and care of these devices is crucial for fostering a sense of control and reducing anxiety.
Moreover, the seamless integration of implantable catheters into the treatment plan enhances overall therapy adherence and contributes to a more streamlined chemotherapy experience.
The Bard PowerPort, a widely used implantable catheter device, has become a focal point in the realm of chemotherapy care. Manufactured by Bard Access Systems Inc., this device facilitates intravenous delivery of fluids, including chemotherapy medications. However, recent lawsuits have raised concerns about potential complications, including migrations, fractures, infections, and blood clots associated with the Bard PowerPort.
Allegations suggest that these complications may lead to severe injuries and, in some cases, even death, prompting affected individuals to seek compensation for damages. According to TorHoerman Law, lawsuits claim that Bard had knowledge of these issues but failed to adequately inform the public.
As the number of Bard PowerPort lawsuits continues to rise, the prospect of settlement negotiations looms large in the legal landscape. Plaintiffs, alleging serious injuries caused by the device, eagerly await resolution through compensation.
However, as of now, no Bard Power Port lawsuit settlement amount has been disclosed. The legal process is still in its early phases, with cases consolidated under multidistrict litigation (MDL) for streamlined proceedings. According to Drugwatch, 8,689 cases have been filed as of October 2025.

Overcoming Financial Barriers to Treatment
Financial constraints can pose significant hurdles in accessing and adhering to chemotherapy regimens. Exploring financial assistance programs and insurance options while advocating for policy changes are vital steps in ensuring equitable access to cancer care.
Healthcare providers and support organizations should proactively communicate available resources to patients, assisting them in navigating complex financial landscapes.
Collaboration between healthcare institutions and advocacy groups can drive systemic changes. It addresses the economic burdens associated with cancer treatment and promotes a more inclusive and accessible healthcare system.
Collaborative Care Teams for Holistic Support
A multidisciplinary approach involving oncologists, nurses, psychologists, and nutritionists is essential. Collaborative care teams can address the physical, emotional, and nutritional aspects of a patient’s well-being, fostering holistic support throughout the chemotherapy journey.
Regular interdisciplinary meetings ensure comprehensive care planning, with each team member contributing expertise to enhance the overall patient experience.
Psychosocial support, nutritional guidance, and pain management strategies are seamlessly integrated into the treatment plan. This creates a supportive network that recognizes and addresses the diverse needs of individuals undergoing chemotherapy.
Paving the Way for Future Innovations
Investments in research and development are crucial for advancing chemotherapy care. From developing targeted therapies to refining drug delivery methods, ongoing innovation holds the promise of improving treatment efficacy. It also reduces side effects and ultimately enhances the quality of life for cancer patients.
Clinical trials exploring novel drugs and treatment modalities contribute valuable data to the scientific community, driving progress in the field. Collaboration between researchers, pharmaceutical companies, and healthcare institutions accelerates the translation of scientific discoveries into practical applications. This brings new and improved chemotherapy options to patients.
The commitment to research and development underscores the ongoing efforts to evolve cancer care, offering hope for more effective treatments in the future.
Final Thoughts
Navigating chemotherapy challenges requires a holistic approach encompassing precision in medication delivery, personalized side-effect management, patient education, and technological innovations. Implantable catheter devices, despite recent concerns, remain crucial for treatment optimization.
Financial barriers highlight the need for advocacy and collaborative efforts to ensure equitable access. The multidisciplinary care approach, coupled with ongoing research investments, promises an evolving landscape of improved efficacy and enhanced patient well-being.
As legal proceedings unfold, a balanced focus on patient welfare and systemic improvements ensures a compassionate trajectory in chemotherapy care.